00389 2 3091 484
00389 2 3091 484
Transposition of the great vessels in a newborn
December 12,2019
Mihail was born on November 19th at the Clinical Hospital Shtip. Immediately after birth, he showed symptoms of congenital heart failure, and at the age of 8 hours he was referred to the University Clinic of Paediatric Diseases, where appropriate care was given.
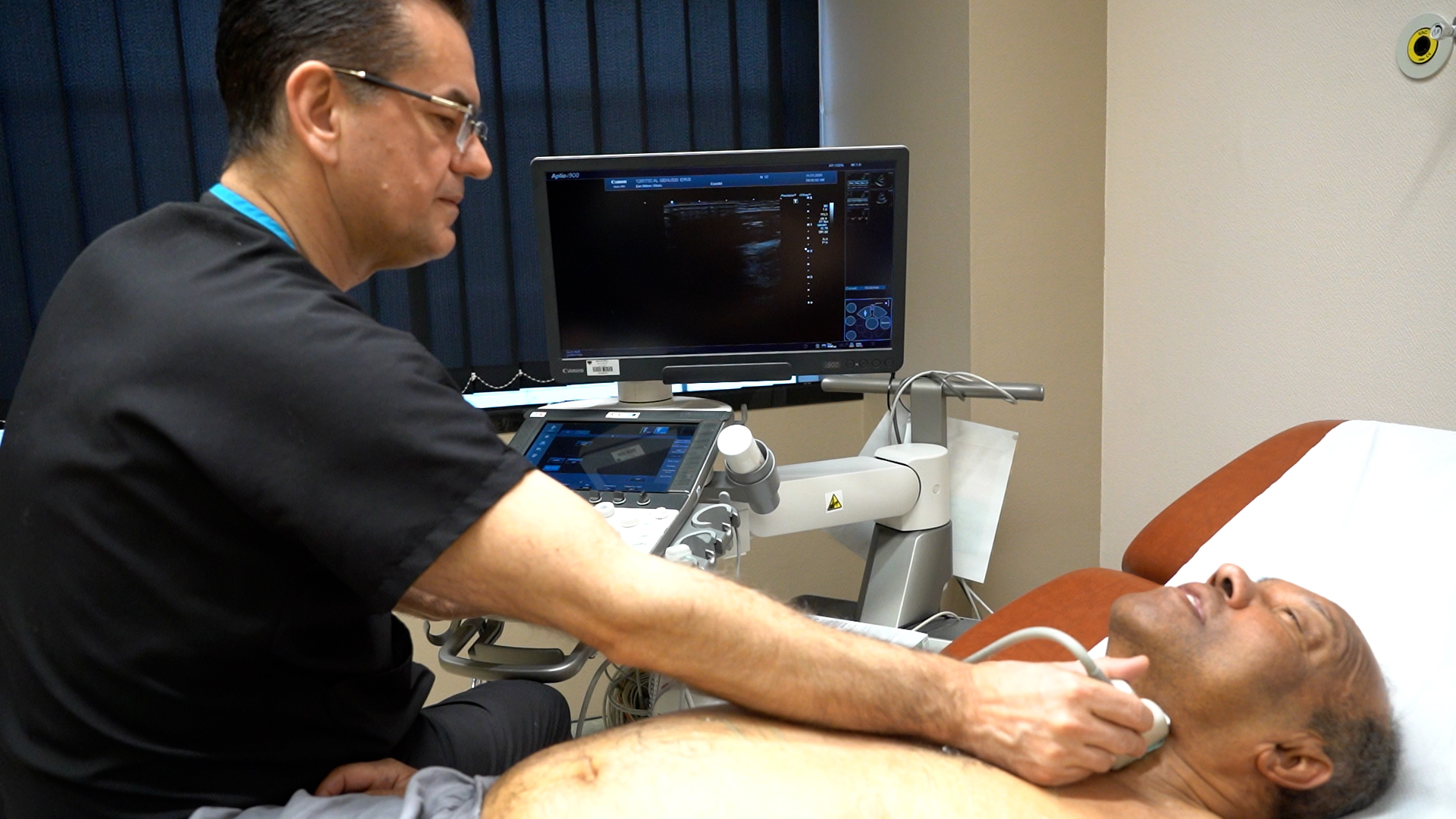
Due to respiratory distress, he was intubated and placed on mechanical ventilation. After performing echocardiographic examination and specifying a defect in favour of transposition of the great vessels, he was given prostaglandin therapy, as well as supportive heart therapy, and he was transferred to Zhan Mitrev Clinic for surgery.
- The newborn arrived in our hospital in a very serious condition, with generalized cyanosis (bruising all over the body), 40% oxygen saturation, shortness of breath and rapid breathing, low blood pressure, signs of heart and kidney failure, a condition requiring urgent cardiac correction. Our doctors also confirmed the congenital heart defect transposition of the great vessels. The moment when the patient arrived was very exciting, as a 4 month old infant with complex heart failure had a surgery, so the period until that surgery was completed was used for urgent stabilization of Mihail’s condition, preoperative protocol preparation by analysing the needed lab tests, X-rays and transfusion analysis. At the same time, the newborn had a specific blood group, O negative, for which blood and blood derivatives had to be provided immediately – explained Dr. Jordanka Madjovska, a paediatrician at our clinic.
The newborn was operated by our team led by Dr. Zhan Mitrev, and the surgery lasted 4 hours. An arterial switch operation was performed, which means suturing the large blood vessels at the appropriate outlet, more precisely, the aorta is sutured to the left ventricle outlet and the pulmonary trunk to the right ventricle outlet. Thr coronary blood vessels from the new aorta were also sutured, which means a complete correction of the congenital heart defect was made.
The postoperative period generally passed without complications, with regular echocardiography examinations and normal cardiac function.
On the 13th postoperative day, the newborn was given to the mother and active breastfeeding began the following day.
Transposition of the great vessels is a congenital heart defect that is part of the group of cyanotic defects with a bidirectional shunt. It is an anomaly where the aorta exits the left ventricle rather than the right one and the pulmonary artery exits the right ventricle rather than the left one. Thus, the blood circulating throughout the body is not oxygenated and the body is not supplied with enough oxygen. This anomaly is life-threatening if proper treatment is not taken immediately. This heart defect is present in 8-10%. It is a ductal-dependent defect, more precisely it is necessary to keep the arterial duct (the artery between the aorta and the pulmonary artery) open. The treatment consists of two options, the palliative option with Rashkind balloon atrioseptectomy – opening a larger aperture between the two atria to mix more blood to get more oxygenated blood with complete correction of the congenital heart defect within a few weeks. The second option is cardiac surgery with complete correction of the heart anomaly – informed Dr. Zhan Mitrev.
This is the second case of such congenital heart anomaly treated in our clinic. The previous one was in August, which is regularly monitored at our institution. The infant Rinisa has an excellent echocardiographic finding now, with excellent progress in weight gain.