What are the first COVID-19 symptoms?
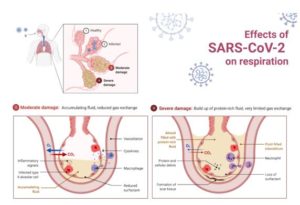
The new coronavirus infection can cause, among other things, fever, cough, and muscle aches. These symptoms can also occur with other viral infections that are characteristic of this autumn period.
What should we pay attention to?
One of the parents’ tasks, given the start of school, is to measure the temperature of their children in the morning before taking them to school / kindergarten.
This is very important because if their temperature is higher than 37.5°C, then they should not enter the classroom / kindergarten and will have to stay at home. In fact, one of the first signs for alert is fever, and a child with a fever may have COVID-19.
Symptoms may appear 2 to 14 days after making contact with an infected person. They may be: temperature higher than 37.5°C, cough, fever, muscle aches, headache, sore throat. Other less common symptoms are gastrointestinal symptoms such as nausea, vomiting or diarrhoea. Some patients lose taste or smell (children may not be able to communicate this feeling). In any case, a temperature higher than 37.5°C, which cannot be reduced by using antipyretics, is the first sign, followed by a cough that is usually dry, persistent and without catarrh.
The earliest symptoms of the new coronavirus are very similar to those of the seasonal flu. Cough, fever and body aches are present in all diseases caused by various respiratory viruses. Among other things, during the flu season, the infection is very common in school / kindergartens, especially among the youngest ones, because the children spend a lot of time together in the same room.
In general, with flu there is a sudden temperature rise of more than 38°C accompanied by at least one general symptom (malaise and fatigue, headache and muscle aches) and at least one respiratory symptom (cough, sore throat and shortness of breath). In fact, it is impossible to distinguish the symptoms of COVID-19 from the flu symptoms.
The only way to get a definite diagnosis of COVID-19 is to take a swab.
How to behave in case of suspicious contacts?
If there is a suspicion that the child has made a close contact with a confirmed or probable case of COVID-19 in the previous 14 days after the onset of the first symptoms, it is important to stay home and contact a pediatrician who will identify the symptoms and if necessary perform the necessary tests (nasopharyngeal swab). It is essential to follow the network of contacts: classmates, teachers, anyone the child contacted.
By probable COVID-19 case we mean:
- a person living together with someone with COVID-19
- a person who has had a direct physical contact with someone with COVID-19
- a person who has had a direct unprotected contact with secretions from someone who has COVID-19
- a person who has had a direct contact (face to face) with someone who has COVID-19, at a distance of less than 1-2 meters, for more than 15 minutes, without a mask
- a person who has been indoors (for example, a classroom, a meeting room, a hospital waiting room) with someone with COVID-19 for at least 15 minutes, at a distance of less than 1-2 meters, without a mask.
What should parents do if the child is tested positive?
With the start of schools / kindergartens, the child may be tested positive for the new coronavirus. If this happens, do not panic. It is important to know the duration and characteristics of the COVID-19 disease.
This disease in children usually lasts shorter. This is based on previous experiences with this infection as well as the fact that in many children the infection has not caused any symptoms (it is asymptomatic), but even when it causes a disease, the symptoms are usually mild or moderate such as cold, cough and mild fever. If present, the symptoms tend to disappear within a week or two. On average, the disease lasts four or five days.
However, very often the symptoms are underestimated and this leads to a delayed diagnosis. Sure, with the start of school, children will have episodes of fever and cough, and it will be difficult to tell right away if it is COVID-19 or some other seasonal infection.
It is important for the parents to contact a pediatrician who will identify the symptoms and, depending on their severity, make the necessary tests, especially a nasopharyngeal swab. At our hospital, we have tests for detection of the most common viral infections this season, including the coronavirus. If a child is diagnosed with COVID-19, all previous contacts should be traced to stop the transmission. After the child is examined and a swab is taken, the doctor will assess whether hospitalization is needed or the child can be monitored at home through a special COVID-19 monitoring platform that our hospital has. After a 14-day home isolation, the child can safely return to school without symptoms and with negative test.
How long does it take to be COVID-19 negative?
Clinical recovery in children is very fast, except in rare cases. However, it takes more time for the child’s body to get rid of the virus (so-called viral excretion). In some cases, the virus triggers a very rapid immune response that allows children to get rid of the virus quickly. In other children, the immune system is not able to recognize the virus so quickly and their immune response is not as efficient and fast and therefore the virus tends to persist in the body for a long time.
What if children are tested positive but are asymptomatic?
Children (but adults too) can be asymptomatic, i.e., infected with the virus, but not showing any symptoms, and thus they can transmit the disease to others.
The situation becomes complicated schools / kindergartens, a place where children and young people have to spend several hours together. Having a potential source of infection in the classroom and not being able to identify it is a risk for all students to get sick. Such cases are rare but should not be ignored.
How to protect ourselves?
It is currently impossible to detect asymptomatic adults and children unless a nasopharyngeal swab is taken repeatedly.
It is therefore necessary to try to limit the infection in children and at the same time allow them to return to school, their everyday life and games as safely as possible by adhering to the recommended protection measures – keep distance, wash hands and wear masks where recommended.
Prim. Blagica Mancheva, MD
Specialist in pediatrics
Breast cancer is curable if diagnosed early
Breast cancer is the second most commonly diagnosed cancer in women, after skin cancer, and the second most common cause of cancer death, after lung cancer.
Statistics show that the incidence of the disease in the last 30 years is growing globally, i.e., 3.1% per year, and mortality varies.
Studies show that on average, 1 in 8 women will develop breast cancer in their lifetime. About two-thirds of women are over 55, and the rest are between 35 and 54.
Postmenopausal women are twice as likely to develop cancer if they have obesity problems.
WHAT IS BREAST CANCER
The direct cause for a normal cell to become malignant has not yet been fully elucidated, but the genes involved in cell development, growth, and death are responsible for that change. There is a balance between cell’s growth and death. With the loss of this balance, uncontrolled proliferation of biologically altered cells occurs. If these cells travel to places where they are not usually found, we say that the cancer is metastatic.
Breast cancer usually starts in a limited region of the milk-producing glands (lobular carcinoma) or in the ducts (ductal carcinoma) that carry milk to the nipple. It can grow in the breast and spread to nearby lymph nodes or through the bloodstream to other organs.
Men can get breast cancer, but only 1% of all cases are of this type.
Symptoms
What are the early symptoms of breast cancer?
- Changes in the nipple shape
- Chest pain, especially after menstruation cycle
- A lump that does not disappear after menstruation cycle
- Red or brown nipple secretion
- Unexplained redness, swelling, inflammation of the skin, itching or rash
- Swelling or lump around the armpits or at the end of the breast.
Risk factors
There are several factors that increase the risk of this disease. Unfortunately, we cannot influence the most important ones:
Age group – the older the woman, the greater the risk
Family medical history – women whose sister, mother or daughter have already had the disease
Hereditary factor – about 5 to 10% of all breast diseases are caused by a hereditary factor
First menstruation at the age of 12 and last after the age of 55
Women who did not give birth, or gave birth after the age of 30
Hormone therapy
Excessive alcohol consumption
Overweight.
Prevention
Pay more attention to a healthy and varied nutrition
Physical activity
Avoid hormonal preparations.
Early detection of the disease
Self-examination
Mammography of patients over 40 years or earlier – by decision of a specialist radiologist
Breast echotomography
Breast MRI.